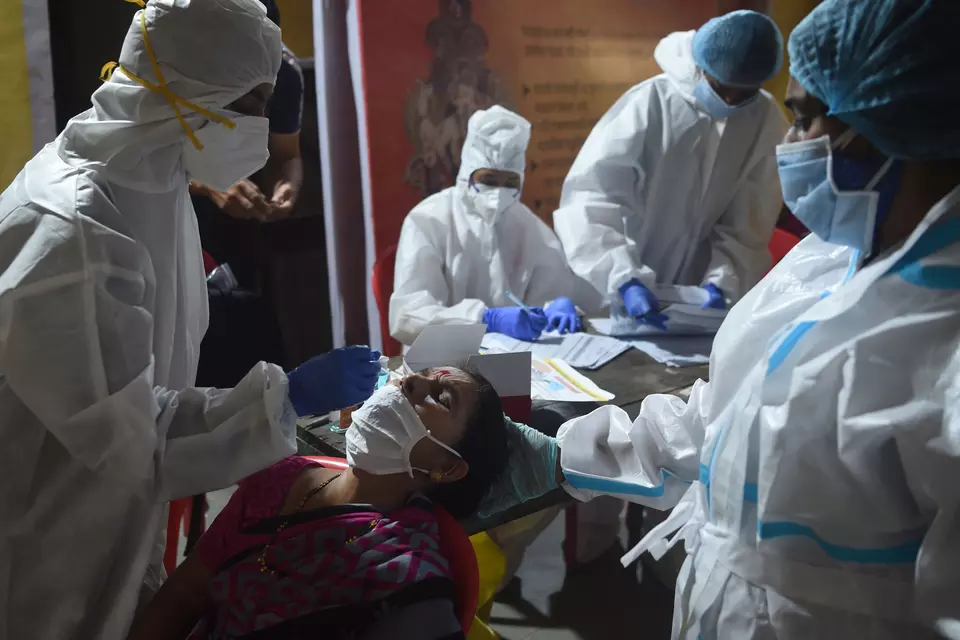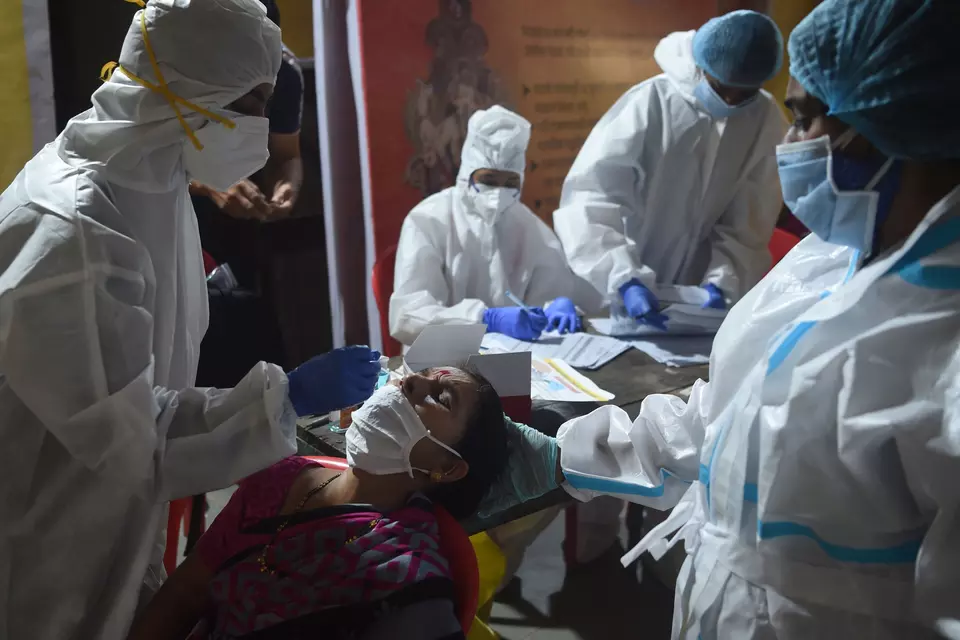
The Covid-19 pandemic claimed millions of lives and exposed severe limitations in global health systems, particularly in India, that officially recorded over half a million deaths. This crisis strained the country’s healthcare infrastructure, revealing glaring inadequacies in its preparedness. It underscored the urgent need for a comprehensive strategy to manage future health crises, particularly pandemics, while highlighting the absence of a robust legislative framework for handling such emergencies. India relied on outdated laws that proved utterly inefficacious during the crisis. In response to this lack of readiness, Niti Aayog recently released a report entitled “Future Pandemic Preparedness and Emergency Response: A Framework for Action”, emphasising the need for legal and policy reforms.
Infrastructure and Financial Deficits: Addressing legislative gaps is critical, but it must coincide with strengthening India’s healthcare infrastructure and ensuring adequate financial support. Currently, India’s healthcare system remains underfunded compared to global standards. The Union Budget for FY 2024-25 allocated ₹90,958.63 crores (around 0.27 per cent of GDP) to the ministry of health and family welfare, significantly lower than allocations in other nations: Malaysia (8.5 per cent of GDP), Russia (10.2 per cent), South Africa (15.3 per cent), the United Kingdom (19.7 per cent), and the United States (22.4 per cent).
Even when combining Union and state health expenditures, India’s total health spending is approximately 1.9 per cent of GDP for FY 2024, falling short of the National Health Policy’s target of 2.5 per cent for 2025. This persistent underinvestment hampers the development of a robust health system capable of effectively managing emergencies.
The Niti Aayog report calls for greater investment, particularly in rural areas, to address the significant healthcare infrastructure deficit. While the private sector provides around 1,185,242 beds, the public sector lags behind with approximately 713,986 beds, resulting in fewer than 1.4 beds per 1,000 people, well below the World Health Organisation’s recommended three beds per 1,000. Additionally, the doctor-to-population ratio is roughly 1:1,511, falling short of the WHO benchmark of 1:1,000. Despite recent increases in the number of doctors at primary health centres (PHCs), many PHCs still lack adequate medical staff, with the number of auxiliary nurse midwives (ANMs) decreasing from 213,467 in 2014 to 207,604 in 2022, signalling a critical gap in frontline healthcare personnel. The primary health centres (PHCs) and community health centres (CHCs), especially in rural India, suffer from a chronic lack of doctors and other medical professionals with high-end equipment lying unutilised. A classic case in point was a dialysis machine that I gave to a CHC in Garhshankar in my former parliamentary constituency of Sri Anandpur Sahib in 2020 that despite being installed and made operational has not been utilised perhaps even once as there is an inadequacy of trained staff to run it.
Inadequacies in India’s Legal Framework: During the Covid-19 crisis, the Indian government relied on the Epidemic Diseases Act of 1897 (EDA) and the Disaster Management Act of 2005 (DMA). However, neither law was equipped to handle a prolonged health emergency. The EDA, a colonial-era statute designed to curb the spread of the plague, is too narrow for today’s complex health challenges. Its outdated provisions offer limited powers to states and lack mechanisms for effective coordination between Central and state authorities. Moreover, the Act does not address crucial aspects such as technology use, digital health records, drug and vaccine distribution, and modern quarantine practices.
The DMA, intended for natural disasters, was used to implement lockdowns and allocate resources during Covid-19. However, its framework is misaligned with managing a prolonged public health emergency. The DMA’s provisions are tailored to sudden disasters like floods, offering little guidance on maintaining public health infrastructure over time. This misalignment led to inconsistencies in enforcing prolonged lockdowns, revealing its inadequacy for handling complex health crises. Interestingly, most of the Covid-19 guidelines issued by the Central government drew their legal sustenance from the Miscellaneous Provisions of the Disaster Management Act of 2005.
Need for a Comprehensive Public Health Emergency Law: The pandemic highlighted the pressing need for a specialised public health emergency law to bridge gaps in the current legal framework. Such legislation would establish a clearer roadmap for managing health emergencies, delineating the roles and responsibilities of Central, state, and local authorities to ensure seamless coordination. The absence of such a structure during Covid-19 resulted in confusion and administrative lapses, compromising response efficiency.
Another critical aspect is data sharing and transparency. One of the biggest hurdles during the pandemic was the lack of real-time, accurate data, hampering decision-making at every stage. A dedicated public health emergency law should establish clear protocols for data collection and dissemination, ensuring that key metrics such as case numbers and resource availability are tracked and shared in real-time. This would enable informed and timely decisions during health crises.
Incorporating modern technology is crucial. The next era of pandemic preparedness will rely significantly on digital tools like contact tracing platforms, AI for outbreak prediction, and telemedicine for remote patient care. During Covid-19, these technologies were deployed only in a fragmented manner. A robust public health emergency law should ensure that digital innovations are integral to the national response framework.
Bridging the Legislative Gaps in Pandemic Management: India’s struggle during Covid-19 exposed shortcomings in its legal framework for addressing modern pandemics. This legislative gap impacts the coordination, transparency, and efficiency required to handle public health emergencies effectively. To bridge this gap, India needs a dedicated Public Health Emergency Management Act (PHEMA) that goes beyond existing statutes to encompass modern technology, data transparency, and clearly defined roles across all levels of government.
The Niti Aayog’s report emphasises the need for a law that grants special powers to manage health emergencies comprehensively. Such legislation should establish public health cadres at national and state levels, creating a lead agency responsible for implementing emergency measures. This would enable an agile response, ensuring no time is lost in containing outbreaks and building a trained standing workforce for future emergencies.
Countries like the United States, the United Kingdom, and Canada already have comprehensive legal frameworks for managing public health crises. A similar PHEMA in India, equipped with special provisions, would enable priority action in critical areas: Strengthening pandemic preparedness expertise, regulating ports of entry, coordinating interstate movements, and managing misinformation. It would also facilitate the faster development and approval of diagnostics and vaccines, expedite emergency procurement, and enhance international coordination for global health threats.
Combining such legislation with stronger infrastructure and greater financial investments will ensure that India is better prepared for future pandemics, building a resilient public health system capable of responding swiftly and effectively to any health crisis.
Finally, what has completely been buried in the aftermath of the Covid-19 crisis was the dubious role of the World Health Organisation (WHO) in the opening days of the pandemic. The WHO acted more like an apologist for China rather than a global health coordination agency. The role of the WHO has never been audited by its sovereign stakeholders. It is a necessity that has not yet lost its purpose.