Patching legacy systems is a pain, but healthcare IT leaders and workers do it every day. Is complete modernization of health IT far away?
Artificial intelligence is exploding in healthcare. There have been a lot of administrative uses for it; far fewer clinical deployments yet. What could happen to drive routine use of AI by hospitals and health systems into the mainstream?
Everyone in healthcare knows value-based care is slowly taking hold in the industry. But what can make it the industry standard? AI perhaps?
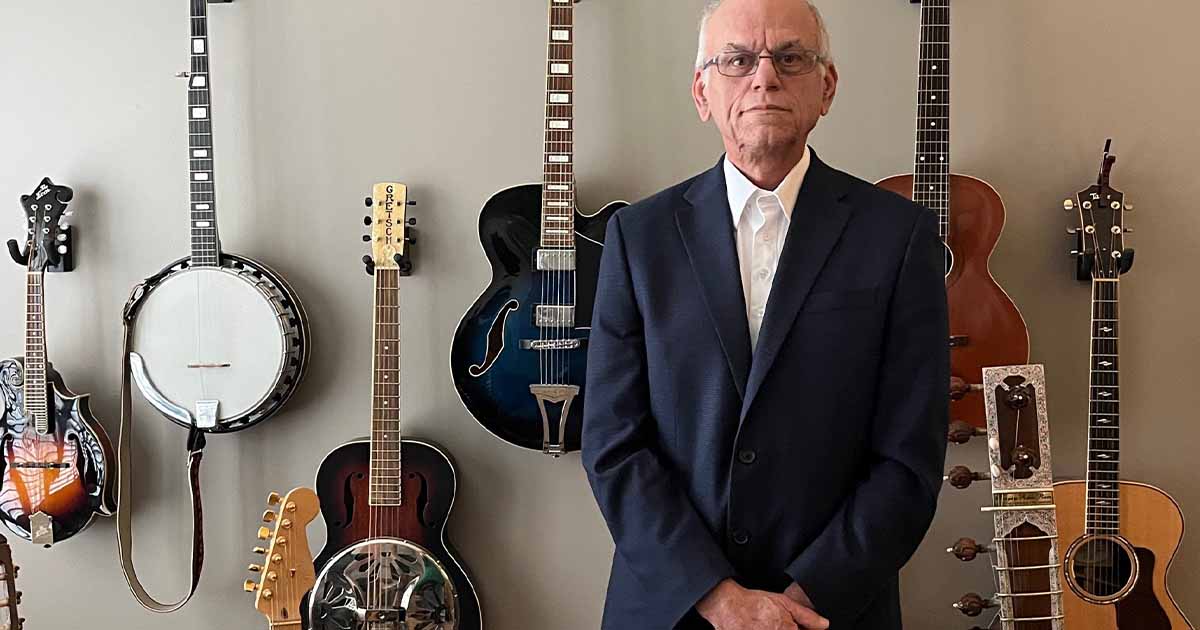
Robert Connely has answers for all three of these questions – and he says change for all three will happen this year.
Connely is the global industry market leader for healthcare at Pega, a vendor that specializes in enterprise AI decision making and workflow automation. He has more than three decades of entrepreneurial, innovation and strategic leadership experience in global organizations such as McKesson and Aetna and successful health IT start-ups such as Medicity.
‘Reimagine and replace’
Healthcare provider organizations this year will abandon the “wrap and renew” approach to legacy systems in favor of targeted “reimagine and replace” strategies, Connely predicts.
“The shift in 2025 from patching legacy systems to full modernization requires a fine balance,” he said. “The goal is to empower organizations to address complex processes using technologies like AI, driving future value while minimizing the technical debt associated with maintaining legacy systems.
“This transformation is likely to impact two primary areas: the evolution of modernization strategies themselves, and the rise of AI orchestration platforms,” he continued. “These elements are unfolding simultaneously, but a distinct pattern is emerging.”
Modernization has shifted away from the traditional “rip and replace” approach, which swaps outdated systems for newer ones – while effective, this method is highly complex, costly and time-consuming, often taking months just in the discovery phase alone, he added.
“It also often fails to address the intricate processes that businesses now face, such as holistic patient care and provider lifecycle management,” he stated. “Legacy systems were not designed to handle these interconnected workflows.
“A subsequent approach, ‘wrap and renew,’ sought to extend the life of legacy systems by integrating them with newer technologies, enabling their participation in complex workflows,” he added. “However, this approach still leaves technical debt unresolved and just kicks the problem down the road to solve later.”
The emerging trend involves breaking legacy systems into modular components and distributing them across different technology layers, allowing greater flexibility and scalability, he said.
“This is an approach we’re calling ‘rethink and replace,’ and it uses generative AI to quickly and cost-effectively align business and IT to design and automate new workflow improvements,” he said. “This ability extends low code technology allowing organizations to accelerate time to value while reducing development efforts traditionally needed to program AI to perform complex orchestrations.
“AI-powered orchestration platforms are a key enabler of this new approach,” he noted. “These platforms connect legacy systems to modern workflows, addressing contemporary business, regulatory and security requirements without requiring costly and cumbersome retrofits. By creating a bridge between old and new, these platforms allow gradual modernization.”
Organizations can deploy modern workflows today while charting a clear path to eventually decommission legacy systems, he advised. The pivotal question then becomes: When does the technical debt outweigh the value of keeping the legacy system?
“By applying these modernization concepts and platforms, organizations will create phased roadmaps that ultimately lead to the retirement of legacy systems as their functions continue to live on and evolve in newer platform environments to meet continually changing needs,” he said.
AI’s future depends on security
The future of AI in healthcare hinges on overcoming security concerns, especially around managing private patent data, and 2025 will be the tipping point, Connely said.
“I see a security breakthrough from two angles: technology and technique,” he predicted. “Currently, most AI in automation and decision making relies on statistical AI to predict, decide and automate workflows. Security concerns focus on model usage and auditing outputs to track behavior, enhance performance, identify biases and ensure responsible use.
“On the technology side, barriers to AI adoption include securing data for symbolic AI models, like generative AI, and effectively managing and auditing statistical AI,” he continued. “For generative AI, retrieval-augmented generation frameworks enhance prompts by incorporating private data from information systems.”
This involves breaking data into chunks, vectorizing it and embedding it in the prompt sent to the large language model, he explained. While LLMs can be instructed not to use the data for training, there is a mathematical possibility of decoding the prompt.
“A promising solution lies in homomorphic encryption, a technique that allows data to remain encrypted while being processed by the AI model,” he explained. “With this technology, LLMs can produce augmented responses using encrypted data, which is then decrypted upon return to the source. However, this method is still a few years away from practical implementation. In the meantime, newer approaches are being developed to safely advance AI use.
“One emerging technique involves the adoption of private LLMs,” he added. “Organizations are increasingly building their own vector databases, embedding proprietary data that generative AI can access without exposing it beyond the organization’s security boundaries. This method allows organizations to harness the benefits of generative AI without the risks associated with public tools, such as ChatGPT.”
In addition, developers and integrators are applying AI narrowly within specific process workflows, he noted.
“This focused use limits exposure, reduces security risks and makes it easier to measure value,” Connely said. “By combining these strategies – private LLMs, vector databases and targeted AI applications – executives are finding ways to safely adopt AI while unlocking its potential value.”
AI boosts value-based care
In 2025, AI will be the catalyst that transforms value-based care from a pilot initiative to the standard model across healthcare, Connely predicted.
“Dissatisfaction with U.S. healthcare payers is at an all-time high,” he noted. “The U.S. is unique in having the most technically advanced – and expensive – medical system globally, yet it often serves as a safety net for non-medical challenges such as aging populations, social inequities, environmental factors and behavioral health issues. These realities are driving a shift from fee-for-service models to value-based care contracts.
“VBC fundamentally flips the traditional healthcare model, requiring payers to adopt a more patient- and member-centric approach,” he continued. “This model recognizes that much healthcare utilization is preventable. Often, minor issues – “papercuts” – escalate into costly medical problems when left unaddressed.”
Care management programs have already proven that frequent engagement and proactive interventions can reduce costs by decreasing emergency room visits, hospitalizations and other high-cost services. However, there aren’t enough care managers to scale these efforts across entire populations.
“This is where AI steps in,” Connely said. “AI can augment care management by engaging with members and their broader support networks, including caregivers, family, social services and providers. Through AI-driven orchestration, education and proactive intervention, health systems can address fragmented processes. This extends beyond simple AI chatbots to agentic AI platforms – more sophisticated systems capable of managing complex healthcare challenges and workflows.
“As VBC reshapes the payer’s role, requiring them to take greater responsibility for patient outcomes and journeys, technology becomes a critical enabler,” he continued. “For healthcare payer CEOs, this is top of mind. AI-driven systems allow for better engagement and coordination among providers, members and others in the healthcare ecosystem.”
These advancements are accelerating the shift to VBC by enabling payers to act as true collaborators in improving outcomes while controlling costs, he added.
“Agentic AI also has the potential to address one of the most persistent political divides in U.S. healthcare: the tension between individual and collective solutions,” Connely said. “Traditionally, the inability to make decisions at an individual level has led to healthcare dollars being allocated to broad population cohorts – an approach that is both inefficient and prone to fraud and waste.
“AI changes this dynamic by enabling real-time hyper-personalization,” he added. “It allows payers to analyze individual situations in context and apply tailored rules and interventions that are specific to the individual’s needs at that moment. This approach combines the efficiency of targeted, data-driven care with the fairness of policies designed to benefit everyone.”
By enabling precise, personalized decision making, AI aligns individual care with broader social justice goals, ensuring resources are used more effectively, he said.
“AI technology is evolving rapidly, offering payers new ways to engage with providers, members and social systems,” Connely concluded. “These advancements are laying the groundwork for value-based care to become the standard in U.S. healthcare, delivering on its promise to improve outcomes, reduce costs and transform the system for the better.”
Follow Bill’s HIT coverage on LinkedIn: Bill Siwicki
Email him: bsiwicki@himss.org
Healthcare IT News is a HIMSS Media publication
WATCH NOW: Mount Sinai’s new CDIO offers an inside look at her very full plate